An international team of scientists has identified a long-sought protein that causes liver fibrosis (scarring), paving the way for new treatments. The research was published in the journal Nature Genetics.
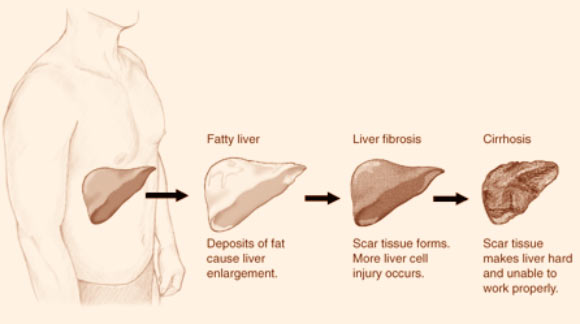
Stages of liver disease. Image credit: National Institute of Diabetes and Digestive and Kidney Diseases.
The team, led by Professor Jacob George and Dr. Mohammed Eslam of the Westmead Institute for Medical Research in Sydney, Australia, has unequivocally shown that variations in the interferon lambda 3 (INLF3) protein are responsible for tissue damage in the liver.
The researchers had previously identified that the common genetic variations associated with liver fibrosis were located on chromosome 19 between the IFNL3 and IFNL4 genes.
In the new study, they analyzed liver samples from 2,000 patients with hepatitis C, using state-of-the art genetic and functional analysis, to determine the specific IFNL protein responsible for liver fibrosis.
They demonstrated that following injury there is increased migration of inflammatory cells from blood to the liver, increasing IFNL3 secretion and liver damage.
Notably, this response is determined to a great extent by an individual’s inherited genetic makeup.
“This was a significant outcome that will help to predict risk of liver disease for individuals, enabling early intervention and lifestyle changes,” said Prof. George, who is the corresponding author of the study.
“We have designed a diagnostic tool based on our discoveries, which is freely available for all doctors to use, to aid in predicting liver fibrosis risk.”
“This test will help to determine whether an individual is at high risk of developing liver fibrosis, or whether a patient’s liver disease will progress rapidly or slowly, based on their genetic makeup.”
“This important discovery will play a vital role in reducing the burden of liver disease into the future,” he said.
“This discovery holds great promise for the development of effective therapeutic treatments for liver disease,” added co-lead author Dr. Eslam.
“There is an urgent need for a safe pharmacologic therapy that can prevent of regress the progression of liver damage. There are currently no treatments available for patients with advanced fibrosis, and liver transplantation is the only treatment for liver failure,” he said.
“Now that we’ve identified IFNL3 as the cause of liver scarring, we can work towards developing novel treatments specifically targeting this gene.”
“This could be medicine targeting IFNL3 that is tailored to an individual’s genetic makeup, but could also include modifying usual treatment depending on whether a patient has IFNL3 risk genes.”
“These outcomes fulfill several promises in the modern era of precision medicine,” Dr. Eslam said.
“Firstly, it brings us closer to the goal of personalized medicine. Secondly, we have a better understand of biology and the way the human body works. Finally, we are a step closer to developing novel potential treatments for liver disease.”
The team will now extend their work to further understand the fundamental mechanisms of how IFNL3 contributes to liver disease progression and to translate these discoveries into new therapeutic treatments.
_____
Mohammed Eslam et al. 2017. IFN-λ3, not IFN-λ4, likely mediates IFNL3–IFNL4 haplotype–dependent hepatic inflammation and fibrosis. Nature Genetics 49: 795-800; doi: 10.1038/ng.3836
This article is based on text provided by the Westmead Institute for Medical Research.







